Living with obsessive-compulsive disorder (OCD) can feel overwhelming. Intrusive thoughts, repetitive behaviors, and constant anxiety can take over daily life. In severe cases, the boundaries between obsessive thoughts and reality may blur, leading many to wonder: Can OCD cause psychosis? While OCD itself does not directly cause psychosis, the two conditions can overlap, and in some situations, symptoms may appear similar. Understanding the differences and connections is essential for proper diagnosis and treatment.
What Is OCD, and How Does It Affect Mental Health?
OCD is a mental health disorder characterized by:
- Obsessions — intrusive, unwanted thoughts, images, or urges that cause anxiety or distress.
- Compulsions — repetitive actions or mental rituals performed to relieve anxiety or prevent a feared outcome.
Most people with OCD are aware that their fears are irrational, which is called insight. This awareness is an important distinction between OCD and psychotic disorders, where insight is often lost.

What Is Psychosis, and How Does It Differ From OCD?
Psychosis refers to a group of symptoms where a person partially or fully loses touch with reality. Common signs include:
- Delusions — fixed false beliefs that are not supported by evidence.
- Hallucinations — hearing, seeing, or sensing things others do not.
- Disorganized thinking — difficulty following logical thought patterns.
Unlike OCD, psychosis is not a single condition but a symptom that can occur in schizophrenia, bipolar disorder, major depression, or as a result of substance use or medical conditions.
OCD vs Psychosis: Understanding the Key Differences
While OCD and psychosis can look similar in severe cases, there are clear differences:
- Insight: People with OCD usually know their thoughts are irrational, while those experiencing psychosis fully believe their delusions are real.
- Response: OCD involves compulsions to neutralize intrusive thoughts, while delusional beliefs typically don’t lead to ritualized behaviors.
- Control: Individuals with OCD actively resist their obsessions, whereas people with psychosis rarely see a need to challenge their beliefs.
However, some severe cases involve OCD with poor insight, where obsessions become so convincing that they resemble delusions.
Can OCD Cause Psychosis or Psychotic-Like Symptoms?
Is there such a thing as OCD-induced psychosis? No, OCD does not directly cause psychosis, although research shows that a small percentage of individuals with OCD also experience psychotic symptoms. This overlap is sometimes referred to as “OCD with psychotic features” or schizophrenia with co-occurring OCD.
In these cases:
- Obsessive thoughts may evolve into fixed beliefs that mimic delusions.
- Intrusive fears can feel indistinguishable from hallucinations or paranoia.
- Both OCD and psychosis symptoms may occur simultaneously, requiring a careful diagnostic assessment.
When OCD and Psychosis Symptoms Overlap
Certain situations make it harder to distinguish between OCD and psychosis:
- Absent insight OCD: When a person fully believes their intrusive thoughts are true.
- Postpartum mental health changes: Intrusive thoughts about harm to a baby are common in postpartum OCD, but postpartum psychosis involves hallucinations and requires urgent medical attention.
- Sleep deprivation and stress: Severe anxiety and lack of rest can make intrusive thoughts feel more real.
- Substance-related triggers: Drugs or medications can worsen OCD symptoms or trigger hallucinations, adding complexity to diagnosis.

Signs It Might Be Psychosis and Not OCD
If you or someone you know experiences any of the following, it may indicate psychosis rather than OCD:
- Strongly believing something untrue despite clear evidence.
- Hearing voices or seeing things others do not.
- Confusion, disorganized thinking, or incoherent speech.
- Extreme changes in behavior, mood, or personality.
- Severe sleep disruption or withdrawal from social interaction.
These symptoms should be evaluated immediately by a mental health professional.
How Mental Health Professionals Diagnose OCD vs. Psychosis
Distinguishing OCD from psychosis often requires a detailed evaluation that considers:
- Insight levels: Whether the person recognizes intrusive thoughts as irrational.
- Thought patterns: Differentiating resisted obsessions from accepted delusional beliefs.
- Behavioral responses: Determining if compulsions are present.
- Medical and psychiatric history: Evaluating contributing factors like trauma, medications, or substance use.
Accurate diagnosis ensures the right treatment plan, especially when symptoms overlap.
Treatment Options for OCD, Psychosis, and Overlapping Symptoms
OCD Treatment
- Cognitive Behavioral Therapy (CBT) with Exposure and Response Prevention (ERP): The gold-standard treatment helps individuals face fears without performing rituals.
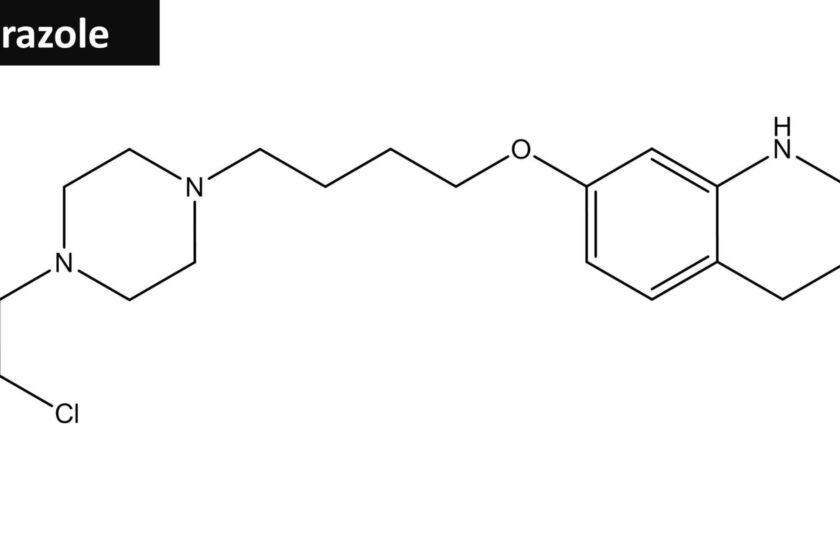
- Medication: Selective serotonin reuptake inhibitors (SSRIs) are highly effective for reducing obsessive thoughts and compulsive behaviors.
Psychosis Treatment
- Antipsychotic medications: These help stabilize delusions, hallucinations, and disorganized thinking.
- Therapy and support services: Once symptoms improve, therapy can focus on managing anxiety, stress, and coping skills.
Treating OCD with Psychotic Features
For individuals experiencing both OCD and psychosis, treatment often combines ERP, SSRIs, and low-dose antipsychotic medications. Careful monitoring by a mental health professional ensures balanced treatment without worsening either condition.
When to Seek Help for OCD or Psychosis Symptoms
If obsessive thoughts, compulsive behaviors, or confusion about reality are interfering with your daily life, you don’t have to navigate this alone. At Experience Structured Living, we provide compassionate, individualized support to help you understand your symptoms and develop a treatment plan that works for you.
Early intervention can make a significant difference. Our team can connect you with experienced clinicians who specialize in OCD, psychosis, and complex co-occurring conditions. Whether you need therapy, medication guidance, or structured support, we’re here to help you take the first step toward stability and relief.
If you or someone you love is experiencing a mental health crisis, call the 988 Suicide & Crisis Lifeline for immediate help.
Final Thoughts: Can OCD Cause Psychosis?
So, can OCD cause psychosis? Not directly, but the two conditions can overlap in ways that make diagnosis and treatment more complex. Understanding the difference between OCD, psychosis, and combined presentations is essential for recovery.
At Experience Structured Living, our mental health housing services in San Diego provide a safe, supportive environment where you can regain control, rebuild confidence, and create a path toward lasting wellness. Our services include assisted living for adults with OCD,
If you’re struggling or worried about a loved one, we encourage you to reach out today. We’re here to answer your questions, discuss your options, and connect you with the care you deserve. Contact us today to get connected with life-changing support.
FAQs: Can OCD Cause Psychosis?
Can stress make OCD symptoms look like psychosis?
Yes, extreme stress can make OCD symptoms more intense and may cause intrusive thoughts to feel more real. While this can resemble psychosis, people with OCD typically maintain some awareness that their thoughts are irrational. If stress makes it hard to tell the difference, a professional evaluation can help.
Is it common to misdiagnose OCD as psychosis?
Yes, it happens more often than people realize. Because severe OCD can involve strong beliefs and overwhelming fears, it can sometimes be mistaken for a psychotic disorder. A qualified mental health professional can perform a full assessment to ensure an accurate diagnosis and the right treatment plan.
Can certain medications trigger psychotic symptoms in people with OCD?
Yes, in rare cases, some medications or substances can increase the risk of psychotic-like symptoms, especially if combined with high stress, lack of sleep, or substance use. If you notice hallucinations, paranoia, or confusion after starting a new medication, talk to your provider right away.
Are hallucinations possible in people with OCD?
While hallucinations aren’t a typical feature of OCD, some people with severe symptoms or co-occurring conditions may experience them. If hallucinations occur, it’s important to seek an evaluation to rule out other underlying causes and ensure proper treatment.
Does having OCD mean I’m at higher risk of developing a psychotic disorder?
Most people with OCD never develop psychosis, but research shows a slightly higher risk compared to the general population. This doesn’t mean psychosis is inevitable. Early treatment for OCD can lower distress and reduce the chances of more severe complications.
Can lifestyle changes reduce the risk of OCD and psychosis symptoms overlapping?
Yes, prioritizing healthy sleep, managing stress, reducing alcohol or substance use, and sticking to a consistent treatment plan can all lower the likelihood of experiencing psychotic-like symptoms alongside OCD. At Experience Structured Living, we work with you to build supportive routines that promote long-term stability.

Dr. Melden earned his Doctorate in Osteopathic Medicine at Philadelphia College Osteopathic Medicine and went to USC Presbyterian Hospital for his residency in Family Medicine. He then completed his Psychiatric residency at the University of California, Irvine and went to UCSD Geropsychiatry pursuing a fellowship. Dr. Melden has over 14 years of experience as a clinician specializing in treating child and adolescent, adult and geriatric clients. He has devoted his life to psychiatry in a variety of different treatment settings including in- patient and out-patient environments. He specializes in the psychiatric evaluation, complementary therapy approaches, and medical management of individuals suffering from mental illness. Currently, he maintains a private practice with Crownview Medical Group in Coronado and Carlsbad, California where he is CEO/President.